


What Is Breast MRI
Why Breast MRI is Done?
The most recent guidelines from the American Cancer Society include “screening MRI with mammography” for certain high-risk women.
1. Women with BRCA1 or BRCA2 mutation
2. Women with a first-degree relative (mother, sister, and/or daughter) with a BRCA1 or BRCA2 mutation, if they have not yet been tested for the mutation.
3. Women who have had radiation treatment to the chest between the ages of 10 and 30, such as for treatment of Hodgkin disease.
4. Women with the genetic disorders Like-Fraumeni syndrome, Cowden syndrome, or Bannayan-Riley-Ruvalcaba syndrome; or those who have a
first degree relative with the syndrome
Some common uses for breast MRI include:
1. Further evaluation of abnormalities detected by mammography
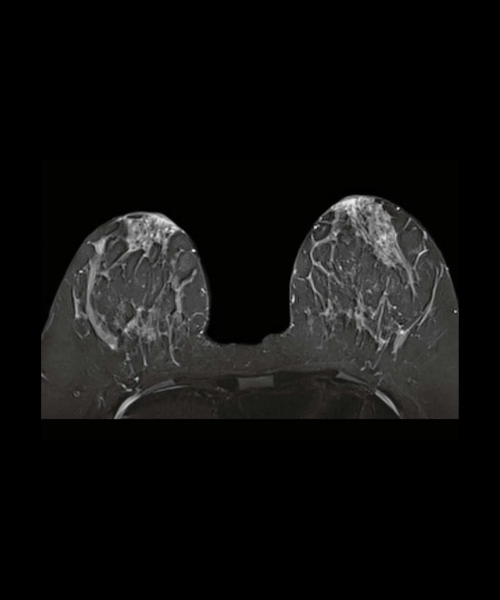
2. Finding early breast cancers not detected by other tests, especially in women at high risk and women with dense breast tissue.
3. Examination for cancer in women who have implants or scar tissue that might produce an inaccurate result from a mammogram. This test can also be helpful for women with lumpectomy scars to check for any
changes.
4. Detecting small abnormalities not seen with mammography or ultrasound (for example, MRI has been useful for women who have breast cancer cells present in an underarm lymph node, but do not have
a lump that can be felt or can be viewed on diagnostic studies)
5. Assess for leakage from a silicone gel implant
6. Evaluate the size and precise location of breast cancer lesions, including the possibility that more than one area of the breast may be involved (this is helpful for cancers that spread and involve more than one area)
7. Determining whether lumpectomy or mastectomy would be more effective.
8. Detecting changes in the other breast that has not been newly diagnosed with breast cancer (There is an approximately 10 percent chance that women with breast cancer will develop cancer in the opposite breast. A
recent study indicates that breast MRI can detect cancer in the opposite
breast that may be missed at the time of the first breast cancer diagnosis.)
9. Detection of the spread of breast cancer into the chest wall, which may change treatment options
Detection of breast cancer recurrence or residual tumor after lumpectomy
10. Evaluation of a newly inverted nipple change.


How do I prepare for a breast MRI?
EAT/DRINK : You may eat, drink and take medications as usual.
CLOTHING : You must completely change into a patient gown and lock up all
personal belongings. A locker will be provided for you to use. Please remove all
piercings and leave all jewelry and valuables at home.
WHAT TO EXPECT : Imaging takes place inside of a large tube-like structure,
open on both ends. You must lie perfectly still for quality images. Due to the
loud noise of the MRI machine, earplugs are required and will be provided.
ALLERGY : If you have had an allergic reaction to contrast that required
medical treatment, contact your ordering physician to obtain the recommended
prescription. You will likely take this by mouth 24, 12 and two hours prior to
examination.
ANTI-ANXIETY MEDICATION : If you require anti-anxiety medication due to
claustrophobia, contact your ordering physician for a prescription. Please note
that you will need some else to drive you home.
STRONG MAGNETIC ENVIRONMENT : If you have metal within your body
that was not disclosed prior to your appointment, your study may be delayed,
rescheduled or cancelled upon your arrival until further information can be
obtained.
Based on your medical condition, your health care provider may require other
specific preparation.
When you call to make an appointment, it is extremely important that you
inform if any of the following apply to you:
You have a pacemaker or have had heart valves replaced
You have any type of implantable pump, such as an insulin pump
You have metal plates, pins, metal implants, surgical staples or aneurysm
clips
You are pregnant or think you might be pregnant
You have any body piercing
You are wearing a medication patch
You have permanent eye liner or tattoos
You have ever had a bullet wound
You have ever worked with metal (for example, a metal grinder or
welder)
You have metallic fragments anywhere in the body
You are not able to lie down for 30 to 60 minutes.
What happens during a breast MRI?
MRI may be performed on an outpatient basis or as part of your stay in a
hospital. Procedures may vary depending on your condition and your doctor's
practices.
Generally, MRI follows this process:
1. You will be asked to remove any clothing, jewelry, eyeglasses, hearing
aids, hairpins, removable dental work, or other objects that may interfere
with the procedure.
2. If you are asked to remove clothing, you will be given a gown to wear.
3. If you are to have a procedure done with contrast, an intravenous (IV) line
will be started in the hand or arm for injection of the contrast dye.
4. You will lie on a scan table that slides into a large circular opening of the
scanning machine. Pillows and straps may be used to prevent movement
during the procedure.
5. The technologist will be in another room where the scanner controls are
located. However, you will be in constant sight of the technologist
through a window. Speakers inside the scanner will enable the
technologist to communicate with and hear you. You will have a
communication ball so that you can let the technologist know if you have
any problems during the procedure. The technologist will be watching
you at all times and will be in constant communication.
6. You will be given earplugs or a headset to wear to help block out the
noise from the scanner. Some headsets may provide music for you to
listen to.
7. During the scanning process, a clicking noise will sound as the magnetic
field is created and pulses of radio waves are sent from the scanner.
8. It will be important for you to remain very still during the examination, as
any movement could cause distortion and affect the quality of the scan.
9. At intervals, you may be instructed to hold your breath, or to not breathe,
for a few seconds, depending on the body part being examined. You will
then be told when you can breathe. You should not have to hold your
breath for longer than a few seconds.
10. If contrast dye is used for your procedure, you may feel some effects
when the dye is injected into the IV line. These effects include a flushing
sensation or a feeling of coldness, a salty or metallic taste in the mouth, a
brief headache, itching, or nausea and/or vomiting. These effects usually
last for a few moments.
11. You should notify the technologist if you feel any breathing difficulties,
sweating, numbness, or heart palpitations.
12. Once the scan is complete, the table will slide out of the scanner and you
will be assisted off the table.
13. If an IV line was inserted for contrast administration, the line will be
removed.
While the MRI procedure itself causes no pain, having to lie still for the length of
the procedure might cause some discomfort or pain, particularly in the case of
a recent injury or invasive procedure such as surgery. The technologist will use
all possible comfort measures and complete the procedure as quickly as
possible to minimize any discomfort or pain.

What happens after a breast MRI?
You should move slowly when getting up from the scanner table to avoid any
dizziness or lightheadedness from lying prone for the length of the procedure.
If any sedatives were taken for the procedure, you may be required to rest until
the sedatives have worn off. You will also need to avoid driving.
If contrast was used during your procedure, you may be monitored for a period
of time for any side effects or reactions to the contrast, such as itching,
swelling, rash, or difficulty breathing.
If you notice any pain, redness, and/or swelling at the IV site after you return
home following your procedure, you should notify your health care provider, as
this could indicate an infection or other type of reaction.
Nursing mothers may choose not to breastfeed for 12 to 24 hours after a breast
MRI with contrast.
Generally, there is no special type of care required after a breast MRI scan. You
may resume your usual diet and activities, unless your health care provider
advises you differently.
Your health care provider may give you additional or alternate instructions after
the procedure, depending on your particular situation.


What are the risks of a breast MRI?
There’s very little risk to getting a breast MRI if you and your technologist follow the
safety guidelines. The possible risks are:
Allergy to contrast dye: There’s a chance you might have an allergic
reaction to the contrast dye, but this is rare. Reactions are usually mild, and
your healthcare team will quickly treat it if it happens.
False positives: An MRI is extremely sensitive, so false positives are
possible. This means it may identify tissue as irregular when it’s not. In any
case, if a radiologist sees something in your breast tissue that doesn’t look
normal, they’ll order additional tests to determine exactly what the finding is.
The results of your MRI will be available in your electronic medical records account
(if you have one) and should be available to the healthcare provider who ordered the
test within one to two business days. Your provider will discuss the results with you.
Additional Common Questions
What is the difference between a breast MRI and a mammogram?
Healthcare providers use mammograms and breast MRIs to help detect breast
cancer and other breast abnormalities.
Mammograms are usually the first option for screening and diagnosis of breast
cancer, particularly as mammograms are the only imaging test able to reliably
identify microcalcifications — an early sign of some breast cancers.
